Falls are a major concern for people living with dementia. Because changes in memory, perception, mobility, and overall health increase fall risks, it is vital for care teams to use structured assessments to identify risks early and prevent incidents. One of the most effective tools is a Falls Assessment, which helps caregivers monitor and understand the many factors that contribute to falls.
When Should a Falls Assessment Be Done?
A Falls Assessment should be conducted at key times, including:
• When a person is admitted as a new resident in a long-term care center
• After any change in condition (physical health, functional ability, or cognitive ability)
• Following hospitalization and return to the residence
• With changes in mobility
• With changes in continence, toileting, or elimination
Typically, a nurse completes the formal falls evaluation form, but every staff member should be familiar with it. Since caregivers and aides are often the first to notice changes, understanding the form helps ensure no signs go unnoticed.
Key Elements of a Falls Evaluation Form
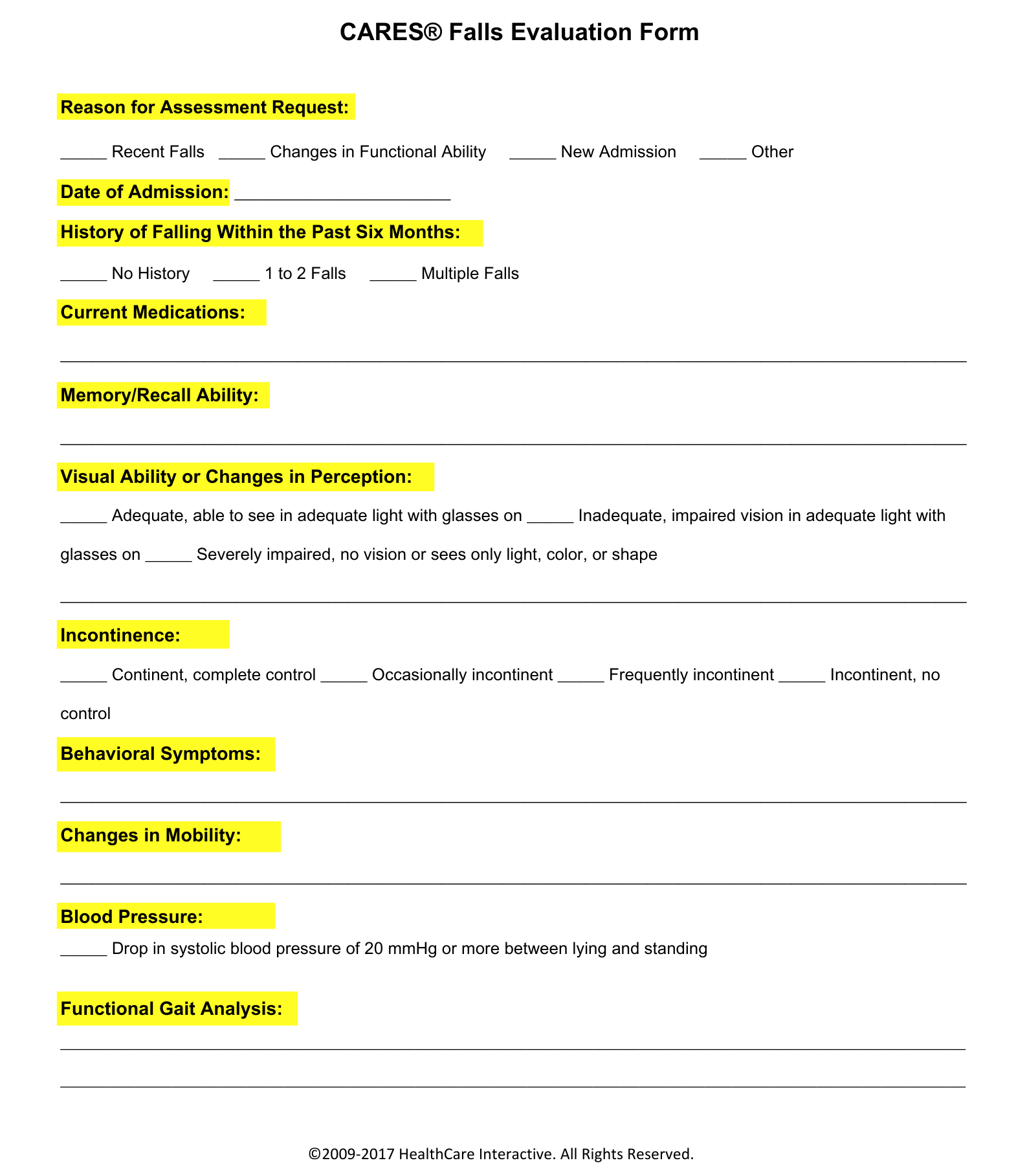
1. Reason for the Assessment
It’s important to document the reason for the assessment—whether it’s a new admission, a change in condition, or post-hospitalization.
2. Date of Admission
Record not just the admission date but also whether the individual is being re-admitted after a hospital stay.
3. History of Falling (Past Six Months)
Patterns of falling provide valuable insight into future risk. Knowing when and how falls occurred can help prevent them.
4. Current Medications
Some medications—or combinations—can increase fall risk by causing dizziness, weakness, or confusion. Staff should monitor closely when a new medication is prescribed.
5. Memory/Recall Ability
People with dementia may forget that they need assistance, or forget to use walkers or canes, increasing fall risk.
6. Visual Ability or Perception Changes
Poor vision can make it difficult to avoid obstacles, navigate steps, or move safely in dim lighting.
7. Incontinence
Rushing to the toilet increases fall risk. Monitoring continence helps in planning safe support.
8. Behavioral Symptoms
Behaviors such as distress, wandering, or agitation can increase fall risks and should be noted.
9. Changes in Mobility
Any reduction in walking ability, transfers, or physical independence must be assessed to adjust support levels.
10. Blood Pressure
Sudden drops in blood pressure while standing up can cause dizziness, leading to falls.
11. Functional Gait Analysis
Observing how a person walks—whether they shuffle, sway, or lurch—helps identify the need for mobility aids or added supervision.
Final Thoughts
Falls can have serious consequences for people with dementia, but structured assessments and continuous observation can significantly reduce risks. Every member of the care team—nurses, aides, and support staff—plays a vital role. By staying alert, understanding assessment tools, and working together, care teams can help keep residents safer, more comfortable, and better supported in their daily lives.
Beyond the Falls Assessment: Continuous Evaluation
Assessment in dementia care should go beyond forms. The CARES® Approach emphasizes ongoing, in-the-moment assessment, which complements structured evaluations like the falls form. Continuous monitoring should include:
• Cognitive health
• Physical health
• Physical functioning
• Safety needs
• Behavioral status
• Sensory capabilities
• Decision-making capacity
• Communication abilities
• Cultural preferences
• Spiritual needs and preferences
Falls put older adults with dementia at serious risk, but proactive assessment and training can make all the difference. Enhance your caregiving skills with CARES® training and certification—now available at 10% off with promo code LaborDaySavings—offer ends September 30, 2025.